Simtegration and Escape Room as Teaching Approaches
Blending Virtual and Hands-On Learning
The College of Western Idaho (CWI) is committed to advancing nursing education through innovation. It consistently seeks to explore new methods to improve learning experiences and better prepare students for real-world clinical practice. As part of this mission, Body Interact Virtual Patients has been integrated into the curriculum, providing a dynamic and interactive environment where learners can experience real-time patient deterioration, collaborate in teams, and make critical decisions—all within a safe and controlled setting.
Educators at CWI follow the “Simtegration” pedagogical approach as a team-based simulation model, combining High-Fidelity Manikins with Virtual Patients. While ‘Simtegration’ does not inherently require a team-based format, this is the chosen method by the institution.
Beyond mastering technical procedures, this method strengthens clinical judgment and decision-making. Rather than simply executing tasks, students are encouraged to analyze patient conditions, anticipate outcomes, and determine the most appropriate interventions.
Body Interact adds an extra layer of realism by enabling learners to witness the rapid progression of a patient’s condition. This requires them to quickly adapt, recognize warning signs, and respond under pressure.

Team-Based Learning Experience
Each simulation runs twice: first, with guided discussions to enhance understanding, and then with minimal instructor intervention. This structure allows participants to demonstrate greater confidence and efficiency in decision-making.
Because all team members manage the same patient, collaboration and real-time communication are essential. Faculty were impressed by the natural teamwork and problem-solving that emerged as students delegated tasks, made critical decisions, and adapted to patient deterioration—both in the manikin-based simulation and the Virtual Patient platform.
According to Professor Jen Mimish, one of the most impactful aspects of Body Interact is the ability for students to “see and hear a patient’s condition change in real-time.” Suppose a healthcare provider delays action or makes an incorrect decision, the patient’s status worsens, forcing the team to adjust their plan immediately. This fosters a sense of urgency and responsibility, mirroring the high-pressure nature of real clinical environments.
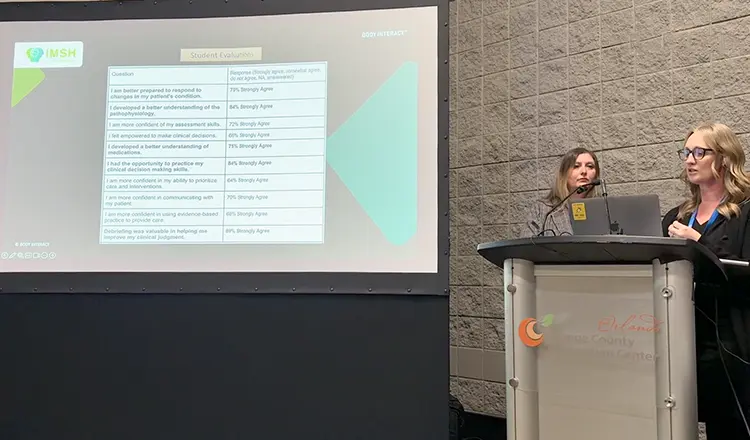
The Impact: Increased Confidence and Preparedness
The impact of this innovative approach has been overwhelmingly positive:
of students reported that they had the opportunity to practice clinical decision-making skills.
felt empowered to make independent clinical decisions—a critical factor in building confidence before entering the workforce.
Pediatric Sepsis Escape Room with Body Interact – Virtual Patients
With the ongoing nursing shortage and limited clinical placement opportunities, educators use creative and effective teaching strategies to better prepare students for real-world challenges.
Recognizing that sepsis is the leading cause of hospital admissions, faculty designed the Pediatric Sepsis Escape Room, integrating Body Interact Virtual Patients to enhance the learning experience. This approach helps students internalize the pathophysiology and sepsis protocol in a memorable and engaging way. It allows them to apply clinical knowledge in a high-energy, competitive environment, reinforcing the idea that “early interventions save lives.”
Students solve medical puzzles, numerical and word codes, and other problem-solving challenges during the escape room to progress through the sepsis protocol. Once both teams successfully “escape,” they transition to Body Interact, where they apply their newly reinforced knowledge by managing a pediatric sepsis case in real-time.
From Fun to High-Impact Learning
Faculty were highly impressed with how students collaborated, engaged in professional discussions, and developed strong clinical reasoning and judgment skills. According to Professor Balenda Snow, one of the most valuable aspects of the experience was how students interpreted and analyzed laboratory test values.
With Body Interact’s simulation pause function, educators could stop the case at critical moments, guiding students through lab test interpretation and the physiological changes behind sepsis. This strategy helped learners understand lab trends, recognize warning signs, and quickly apply their knowledge in clinical practice.
Beyond clinical reasoning, students also showed a strong emotional connection with their virtual patients. They were highly engaged, determined to save the child, and deeply invested in ensuring the best possible outcome. This reaction highlights how virtual patients enhance empathy—a vital skill for future healthcare professionals.
Student feedback reflected the overwhelming success of this innovative learning experience:
felt empowered to make clinical decisions after participating in the escape room and simulation.
reported increased confidence in their ability to prioritize care and interventions.
developed a better understanding of the pathophysiology of Sepsis.
By merging game-based learning with virtual patient simulation, nursing educators have discovered a highly effective approach to reinforcing critical clinical concepts, fostering engagement, and equipping students with essential decision-making skills. Whether through the Pediatric Sepsis Escape Room or the Simtegration model at the College of Western Idaho, these innovative learning experiences are shaping the next generation of healthcare professionals.