Simulation is challenging instructors to integrate virtual patients into their educational programs. Even though the new generations of learners, and future educators, are born into a world of new technologies, it’s a continuous challenge to implement new technological solutions into a school’s curriculum.
As an answer to that challenge, Lorraine Betts, Professor of Simulation Education at George Brown College, in Canada, hosted a workshop at SIM Expo 2019 and another at IMSH 2020 under the topic of “how to use an interactive digital simulator in a nursing program”.
Simulating one of her classes was the exercise Lorraine decided to do. The congress’ participants embodied the role of students, who eagerly try to solve the clinical case. The nursing educator stayed on her daily role, as a class facilitator.

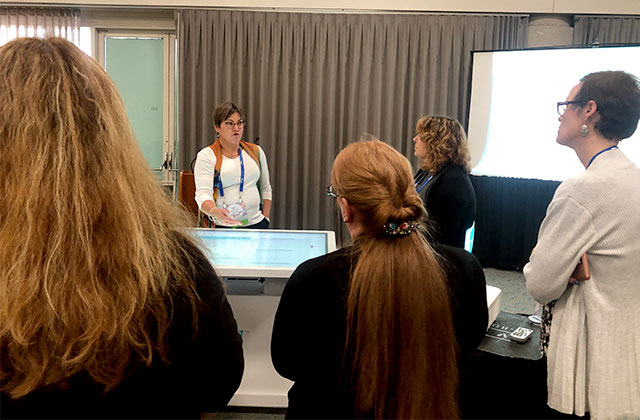
On both workshops, educators took the role of students, by solving and debriefing on a clinical case together
[photos: IMSH workshop]
Dynamic classes with students playing distinct roles
In her classes, Lorraine takes advantage of having a Body Interact table to run a complete scenario and starts the exercise by defining the roles of each student. After a five minutes presentation of the software, students are ready to run a new scenario, related to the topic explored in theoretical classes.
Students take a role and are assigned with specific tasks during the simulation
For first year students, a task is assigned to each of them. One student stays with the vital signs monitoring, other focuses on dialoguing with the patient, while the other colleague manages the physical examination. As a team it is essential to articulate individual intentions with the group’s decisions.
For the higher levels of studies, Lorraine assigns a team leader, who has the duty of driving the team but without taking direct actions on the patient. The remaining members are assigned with specific tasks, such as taking over the interventions, calling for another specialist, if needed, and managing the drugs administration.
The role of an educator
As a facilitator Lorraine focuses on the students’ decisions, attitudes and actions. After all, all the Body Interact scenarios are pre-configured and the outcomes from any action or exam requested are immediately provided by the software.
With the pause button, every time the facilitator recognizes an important step, she is able to stop the case, review the actions made so far and ask the team leader what the team wants to do next.

The pause button allows educators to ask students questions without the patient deteriorating
In case they are struggling to decide what to do and what course to take, Lorraine suggests the following questions:
- What do we know about this patient?
- What data can we extract from that information?
- What do you want to do now?
At the same time a team is running a case, the other students are observing their colleagues’ performance and doing the mental exercise of questioning themselves: How would I do it? Would I make the same decision? What would I make differently?
What can you take away from what you have learned today?
Clinical reasoning is defined by the literature as the process in which nurses “collect cues, process the information, come to an understanding of a patient problem, plan and implement interventions, evaluate outcomes, and reflect on and learn from the process”.
For this reason, nursing students need to follow the step by step framework defined by the guidelines. As a teacher, she needs to direct them to the learning objective.
More than judging or evaluating students’ decisions, it is important to understand what they are thinking, question them about it and then provide feedback about the outcomes.