Nowadays, for healthcare professionals conceptual knowledge and clinical reasoning are two sides of the same coin.
On one side, nurses and doctors are being faced with increasingly complex and rare clinical conditions. On the other side, due to patient’s safety issues, conflicting needs of patients and students and lack of patients, the time of learners spent with patients is decreasing.
For that reason, you are certainly asking yourself: How am I suppose to apply theorical knowledge of foundational courses to clinical problems?
Healthcare professionals will most likely face situations for the first time and not be trained to solve it, however if during their graduation years, they keep improving their critical thinking, decision making and teamwork skills, success is closer to be achieved.

Think and act like a real professional
To tackle the current demands, healthcare training facilities and schools have been adopting different educational approaches, namely by integrating virtual patients in the curriculum. This approach provides a number of benefits like the standardization of clinical teaching, facilitation of learning and providing a transformative learning experience (Imam et al., 2016)
Virtual Patients not only teach core knowledge, but can also be an effective tool to develop communication skills. From multidisciplinary teams to the patients’ family and friends, students are required to learn how to pass a clear message.
After all, as Paulo Martins, intensive care doctor and professor at the Faculty of Medicine of the University of Coimbra, Portugal, mentioned, “a lot of times, doctors have to be the bearers of bad news”.
By focus the learning experience on understanding and applying knowledge rather than memorization and recall, virtual patients challenge students to think and act like real nurses and doctors.
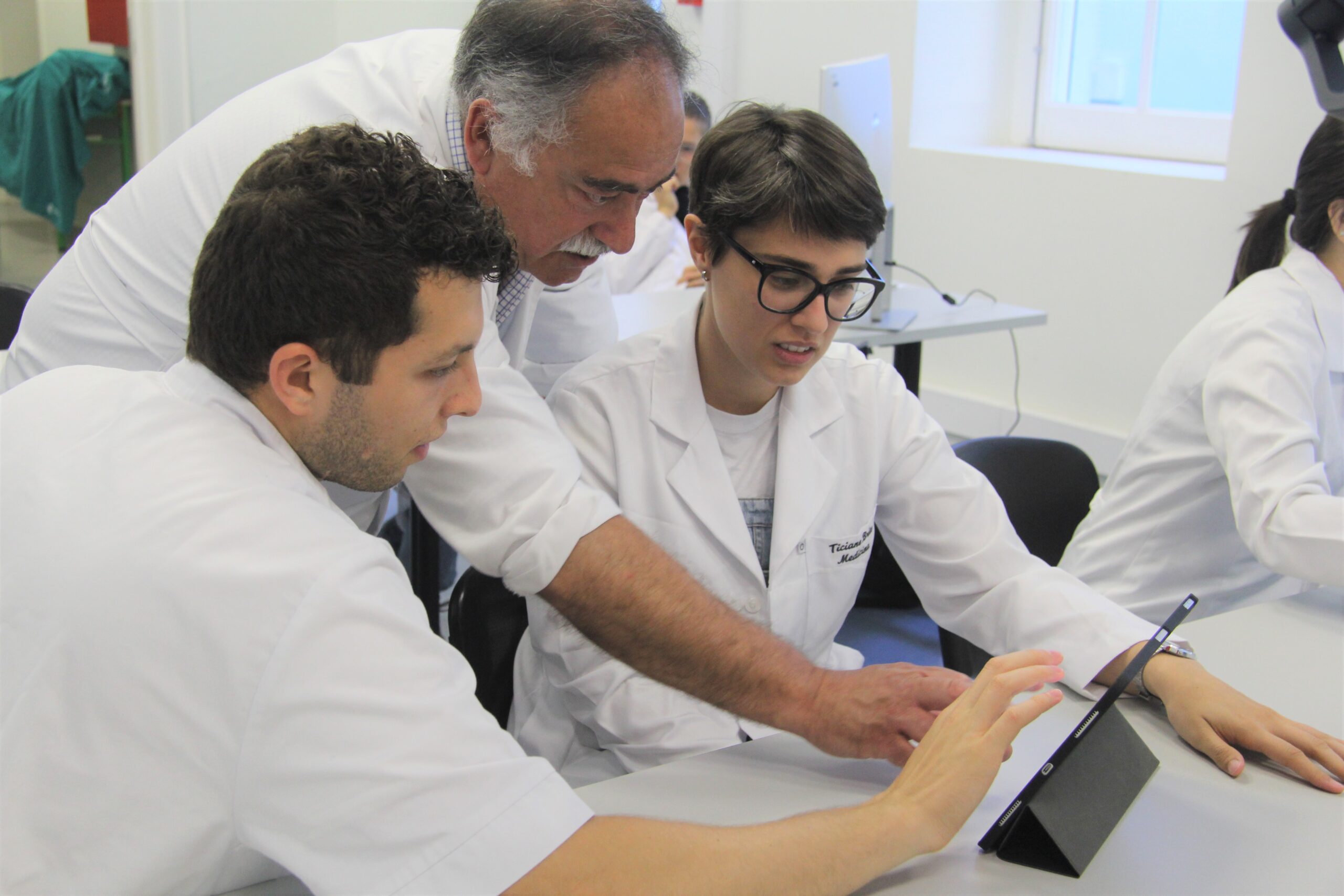
In the opinion of Tina Garza, principal of the Harlingen School of Health Professions, Texas, US, students must “have an idea of the protocol when it comes to do it”. However, the important is not always to recognize step one, two and three, because “sometimes it might be step three and then step five”, she explains.
Connect demands and capabilities
Lorraine Betts, professor of Simulation Education at George Brown College, Canada, explained that Virtual Patients can offer different levels of difficulty according to the levels of learners’ performance.
By applying their own diagnosis and intervention plans, learners are provided with an active learning experience and mentors can provide effective debriefing which helps students identify their strengths and needs for improvement.
Midik and Kartal (2015) explained on their article that mistakes are many times associated with an “inadequate collection of information”. In other words, mistakes are attributed to the lack of experience regarding the diversity of health conditions they have been exposed to during their internships and rotations.

For this reason, working with Body Interact allows educators to standardize educational practice. It ensures the same clinical exposure to attain the same expected competencies to all students, achieving the same level of mastery performance.
After all, as Berman, et.al (2016) stated on their article, students increase their diagnostic skills and knowledge by being educated in a learner-centred classroom and in a virtual patient driven environment.