Pedagogical Approach with Body Interact | Hybrid Simulation
What is Hybrid Simulation?
Different definitions of Hybrid learning can be found in the literature, but our focus this time is on Hybrid Simulation. It is a pedagogical approach that combines multiple simulation resources, such as virtual patients, part-task trainers, high-fidelity simulators, and standardized patients, to create a comprehensive, adaptable, and multi-faceted learning experience. This method leverages the strengths of different simulation modalities to provide learners with a diverse range of experiences, enhancing their clinical reasoning, decision-making, and hands-on skills in a controlled yet realistic environment.
By integrating these various simulation techniques, Hybrid Simulation aims to promote the development of clinical skills and a cohesive learning experience.
Key aspects of Hybrid Simulation:
- Integration of multiple simulation modalities and/or resources
- Combination of diverse clinical skills for development
- Adaptability and flexibility
- Bridging the gap between theory and practice
- Safe and controlled environment for learning
- Learner-centered approach
How can it be applied with Body Interact?
Let’s outline a simple example:
Select a Body Interact scenario that will serve as the unifying resource of the hybrid simulation experience. Then, review the scenario learning objectives, priority actions, and the list of clinical competencies the scenario is designed to develop. All this information can be found in the Body Interact Learning Management System, the Studio, to identify which tasks should be proposed for the exercise.
Among other possible actions that could be integrated into this hybrid simulation experience, imagine this is a hypoglycemia scenario that requires the student to:
- Collect a blood sample
- Prepare medication
- Insert an IV to administer medication
- Complete the patient discharge notes
In this hybrid simulation experience, the student would start the scenario in Body Interact. Whenever one of these actions is initiated, we would pause the simulation after the student makes their decision, and they would then perform the tasks with the appropriate materials and simulators.
From a logistics perspective, this information could be organized as follows:
| Learning goal | Skills and competencies developed | Simulators | Material, medical devices, etc |
|---|---|---|---|
| Diagnose and treat hypoglycemia | Clinical reasoning Decision-making Prioritizing |
Body Interact | Computer or other devices |
| Collect blood sample for analysis | Venipuncture technique Handling equipment Aseptic technique Blood collection techniques Labeling and documentation |
IV arm trainer | Gloves Blood collection supplies |
| Prepare medication | Dosage calculation Selection and preparation of medication Aseptic technique Use of equipment Medication review and validation |
— | Medication preparation supplies Medication storage Simulated medications Medication carts |
| Administer medication | Venipuncture technique Selecting and handling caths and tubes Aseptic technique Confirm patient ID Securing the IV line Medication review and validation Administer medication prepared Assure patient safety |
IV arm | Medication administration equipment IV administration supplies Simulated medications |
| Write discharge notes | Clinical reasoning and judgment Written communication Information management |
— | Electronic health records, paper discharge note template Medical forms and charts |
What are the benefits of using hybrid simulation and combining it with Virtual Patients?

Safe and risk-free learning environment
Students have the opportunity to practice and make mistakes without risking real patients’ safety, creating an ideal setting for building confidence and competence in managing complex clinical situations.
Adaptability and flexibility
Hybrid simulation can be customized to suit various levels of student expertise and learning objectives, allowing professors to adapt scenarios to meet individual or group needs, skill levels, and specialties.
Cost-effective training solution
This pedagogical approach can be a cost-effective solution, as it maximizes the use of simulation resources already available within the institution.
Promotes active and engaged learning
The combination of multiple simulation modalities and the challenges posed to students engages them actively, fostering a willingness to solve the tasks that make up the learning experience.
Hybrid Simulation best practices suggestions:
- Faculty readiness: The level of preparation and experience with the diverse simulation modalities must be considered when implementing this pedagogical approach. The facilitator must be comfortable with the resources in use so they don’t become a barrier to the teaching moment.
- Student readiness: Consider if students have the prior knowledge and skills required to go through the learning experience successfully. If not, consider adjusting the resources being provided, the level of what is expected in terms of outcomes, or providing the basis so that the students don’t get frustrated.
- Learning goals: The different tasks proposed for the hybrid simulation must be lined up with the learning goals defined. Communicate the goals of the learning experience and how they’re aligned with the curriculum.
- Logistics: List the simulators, materials, and all that may be required to conduct the learning experience smoothly.
- Flexibility in execution: Be prepared to modify simulations in real-time based on learner actions or unexpected developments, mirroring the unpredictability of real clinical settings. Keep in mind that Body Interact is a valuable ally for such adjustments. For instance, if a medication is prepared in a different dosage you will be able to reproduce it in the virtual patient!
- Seamless transitions: Ensure a smooth integration between simulation resources. For example, the scenario can start in Body Interact, in which clinical reasoning and decision-making are done, and integrate part-task trainers or manikins, to perform physical tasks lined up with actions conducted in the virtual patient, or preparation of medication that will be administered to the virtual patient, creating a more authentic experience.
- Simulate real-world team dynamics: If possible, incorporate scenarios that require students to interact with multiple healthcare professions, promoting interprofessional education.
- Focus on non-technical skills: Encourage students to practice and develop communication, leadership, and teamwork skills in addition to clinical competencies.
- Assessment: Map and select the multiple methods of assessment most suitable for the skills being developed/assessed, both with formative and summative purposes.
- Feedback and debriefing: Allocate adequate time for feedback and debriefing after the learning experience.
- Encourage reflection: Foster a culture of self-assessment and reflection, encouraging learners to identify their strengths, weaknesses, and strategies for improvement.
By integrating these best practices, hybrid simulation can be a powerful tool in clinical education, offering a comprehensive and realistic learning experience that prepares students for the complexities of real-world patient care.
This approach fosters the development of both technical skills and the human aspects of clinical practice, making it an invaluable asset in training well-rounded healthcare professionals.
Who is using this instructional strategy?
From the feedback we have received from Body Interact users, a couple of institutions are implementing such a modality.
For instance, that can be seen in classes conducted by Prof. Leila Sales from the Red Cross Higher School of Health in Lisbon and in St. Luke´s Medical Center College of Medicine, in the Philippines.
You will be able to review previous posts on this matter by clicking on the links below:
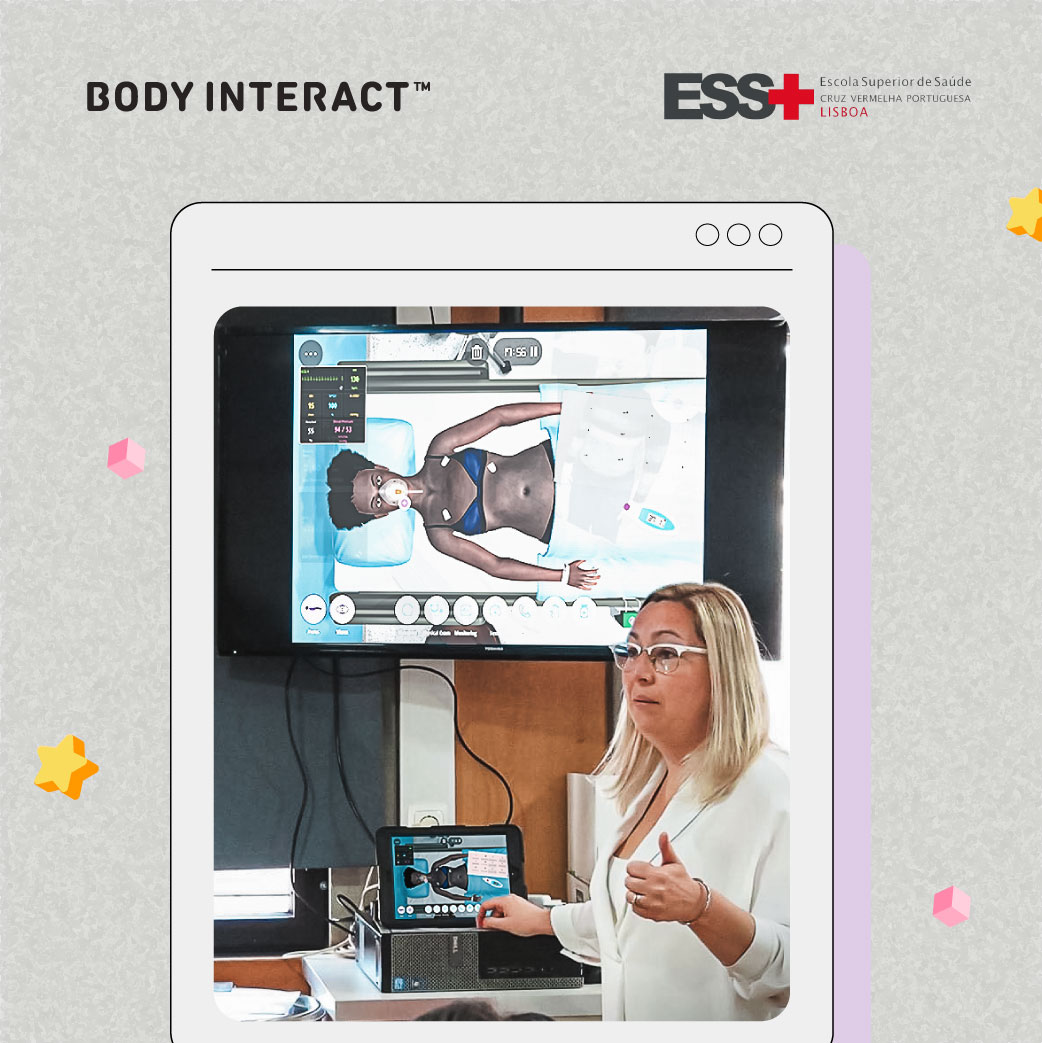
Red Cross Higher School of Health – Lisbon

St. Luke´s Medical Center College of Medicine

Would you like to get to know more about this approach or get the templates we have created for this approach based on Body Interact scenarios? Contact us!
Don’t miss the next Pedagogical Approach with Body Interact!
References
Brown, W.J., Tortorella, R.A.W. Hybrid medical simulation – a systematic literature review. Smart Learn. Environ. 7, 16 (2020). https://doi.org/10.1186/s40561-020-00127-6
Elendu C et all. The impact of simulation-based training in medical education: A review. Medicine 103(27):p e38813, July 05, 2024. | DOI: 10.1097/MD.0000000000038813.
Saichaie, K. (2020). Blended, Flipped, and Hybrid Learning: Definitions, Developments, and Directions. New Directions for Teaching and Learning, 2020(164), 95–104. doi:10.1002/tl.20428.
Vallée A, Blacher J, Cariou A, Sorbets E. Blended Learning Compared to Traditional Learning in Medical Education: Systematic Review and Meta-Analysis. J Med Internet Res. 2020 Aug 10;22(8):e16504. doi: 10.2196/16504.









