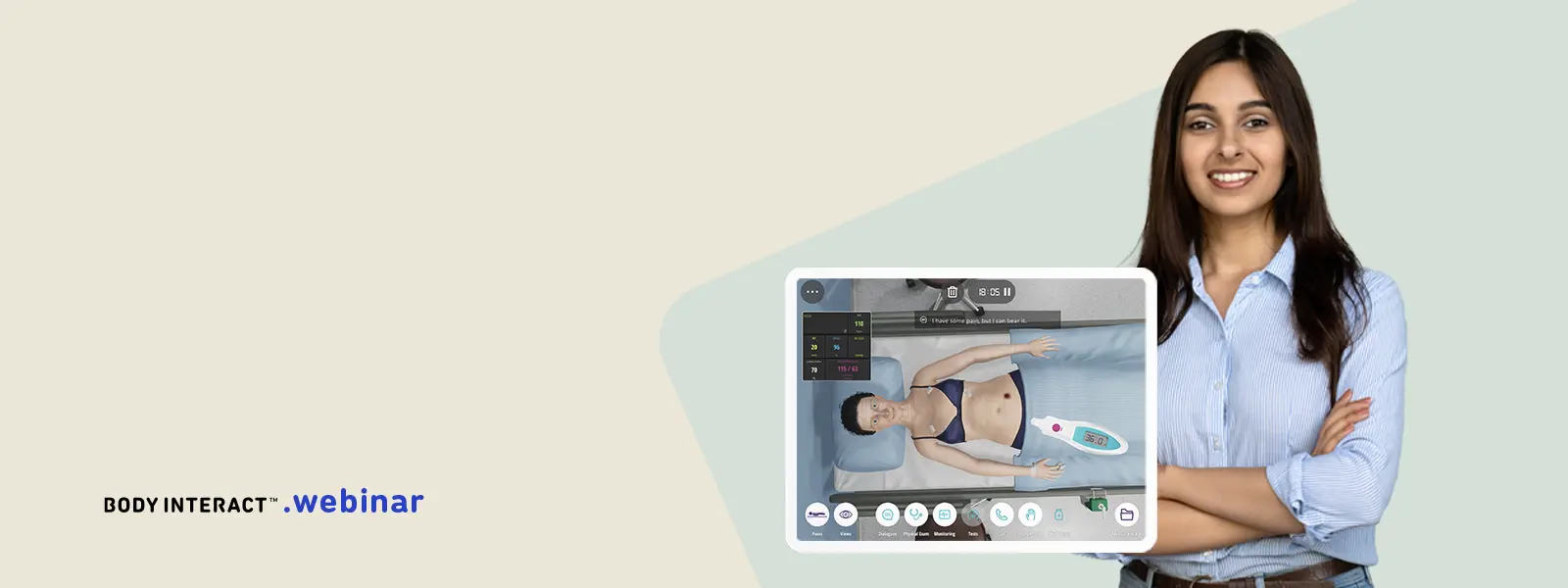
Webinar: The Power of Virtual Patients to Overcome Teaching Constraints
Clinical education stands as the cornerstone of professional health education across disciplines such as Medicine, Nursing, Dentistry, Physiotherapy, and various other healthcare-related professions. Within this educational landscape, students, educators, including both clinicians and non-clinical educators, and institutional boards collectively drive the teaching-learning process in Healthcare-Based Curricula. These stakeholders not only shape the educational journey but also bear significant responsibility for ensuring its effectiveness in Healthcare-Based Curricula.
Healthcare-based curricula cater to both future and current healthcare professionals, thereby making it imperative to address teaching constraints that may hinder their development. The ramifications of such constraints extend beyond individual learners, impacting the broader landscape of public health. Therefore, it becomes paramount to talk about the diverse levels and origins of these constraints, facilitating the exploration of strategies to overcome them. This was our goal with this webinar.
Challenges of Healthcare-Based Education Curricula
The demands within healthcare-based education can manifest in various forms:
Educational Callenges
- Diversity of students
- Ratio student / teacher
- Ratio Student / patient
- Curricular integration
- Faculty resistence
- Standardization
- Evaluation
- Clinical Exposure
- Learning gap
- Budget
Healthcare Challenges
- Load of clinical knowledge
- Rapid evolution of information and guidelines
- Cost reduction drives
- Soft skills
Society Challenges
- Share decision-making
- Access to information
Overcoming teaching-learning constraints in Healthcare-Based Education
In the ever-evolving landscape of healthcare education, the integration of innovative teaching methodologies is paramount to prepare students effectively for the challenges they will face in clinical practice.
One groundbreaking approach gaining traction is the utilization of virtual patients – an innovative and engaging form of simulation that transcends traditional teaching constraints and offers unparalleled opportunities for experiential learning.
Addressing the learning gap
Unlike traditional methods reliant on textbooks and lectures, Body Interact virtual patients immerse learners in dynamic, interactive scenarios where they can apply theoretical knowledge to practical situations in a risk-free environment. This immersive experience not only enhances critical thinking and decision-making skills but also fosters confidence and competence among students, bridging the gap between classroom learning and clinical practice.
Variability of clinical encounters in a standardized way
One of the primary advantages of Body Interact virtual patients lies in their ability to overcome the limitations inherent in traditional clinical training. In conventional settings, students often encounter challenges such as limited access to diverse patient populations, variability in clinical exposure, and ethical concerns surrounding hands-on practice. Virtual patients address these constraints by providing a standardized platform where learners can encounter a wide range of cases spanning different specialties, demographics, and levels. This diversity cultivates adaptability and prepares students to navigate the complexities of real-world healthcare settings with proficiency.
Flexibility
Moreover, Body Interact virtual patients offer unparalleled flexibility in education delivery, accommodating the diverse learning needs and preferences of students. Whether accessed through personal computer or mobile devices, virtual patient scenarios can be selected and tailored to align with curricular objectives, allowing educators to supplement traditional teaching methods or create standalone learning experiences. This versatility extends beyond the confines of the classroom, enabling remote and asynchronous learning opportunities that transcend geographical barriers and time constraints. As a result, students have the freedom to engage with educational content at their own pace, reinforcing learning outcomes and promoting lifelong learning habits.
Risk free teaching and learning
Another compelling aspect of virtual patients is their capacity to simulate rare or high-risk scenarios that may be infrequently encountered in clinical practice but are nonetheless critical for student exposure. From medical emergencies to ethical dilemmas, virtual patient simulations can replicate complex situations with fidelity, enabling learners to develop proficiency in handling challenging cases without compromising patient safety. Additionally, virtual patients offer a controlled environment where students can make mistakes, receive feedback, and iterate on their decision-making process without jeopardizing patient outcomes.
Feedback and Assessment
Furthermore, virtual patients facilitate collaboration by bringing together students to work collaboratively on shared cases. By promoting non-technical skills, such as teamwork and communication, these collaborative learning experiences mirror the interprofessional dynamics of modern healthcare delivery, preparing students to function effectively within multidisciplinary care teams upon entering clinical practice.
In conclusion, virtual patients represent a paradigm shift in healthcare education, offering a transformative approach to teaching and learning that transcends traditional constraints. By providing immersive, flexible, and realistic learning experiences, virtual patients empower students to develop the knowledge, skills, and attitudes necessary for success in clinical practice. As educators and healthcare professionals embrace the power of virtual patients, they pave the way for a future where innovation and excellence converge to shape the next generation of healthcare providers.
Soft Skills
With its built-in real time feedback, Body Interact virtual patients offer an engaging and realistic experience, delivering the required stress that health professionals live when dealing with real patients, and promoting reflection on-actions.
Moreover, Body Interact, provides a diversity of clinical cases and real time feedback on action offering an effective platform to assess skills that traditional assessments often struggle to evaluate efficiently. These skills include clinical reasoning, decision-making, history-taking, prescription, and diagnostic proficiency.
Conclusion
In conclusion, virtual patients represent a paradigm shift in healthcare education, offering a transformative approach to teaching and learning that transcends traditional constraints. By providing immersive, flexible, and realistic learning experiences, virtual patients empower students to develop the knowledge, skills, and attitudes necessary for success in clinical practice. As educators and healthcare professionals embrace the power of virtual patients, they pave the way for a future where innovation and excellence converge to shape the next generation of healthcare providers.
References
Padilha, J. M., Machado, P. P., Ribeiro, A. L. & Ramos, J. L. Clinical Virtual Simulation in Nursing Education. Clin Simul Nurs 15, 13–18 (2018).
Abreu, J. M., Guimarães, B. & Castelo-Branco, M. The role of virtual interactive simulators in medical education: Exploring their integration as an assessment methodology in clinical years. Educacion Medica 22, 325–329 (2021).
Karaduman GS & Basak, T. Is Virtual Patient Simulation Superior to Human Patient Simulation: A Randomized Controlled Study. CIN: Computers, Informatics, Nursing (2022) doi:10.1097/CIN.0000000000000957.
Mestre, A. et al. The impact of small-group virtual patient simulator training on perceptions of individual learning process and curricular integration: a multicentre cohort study of nursing and medical students. BMC Med Educ 22, 375 (2022).