Pedagogical Approaches with Body Interact | Clinical Reasoning Assessment
What is clinical reasoning?
A skill, process, or outcome wherein clinicians observe, collect, and interpret data to diagnose and treat patients.
Daniel et al, 2019
Clinical reasoning is the cognitive process that healthcare professionals use to assess, diagnose, and treat patients. In simpler terms, clinical reasoning is how a clinician thinks through a patient’s case to make safe and effective medical decisions.
It involves several key components.
Key Components of Clinical Reasoning
Clinical reasoning is a multifaceted and integrative process involving several interrelated components:
- Information gathering: The process of collecting the information necessary to develop, generate, or refine hypotheses.
- Hypothesis Generation: The process by which a clinician identifies potential diseases that could account for a patient’s clinical findings.
- Problem Representation: A flexible mental summary that brings together all important elements of a case – such as clinical findings and psychosocial factors.
- Differential Diagnosis: A list of diagnostic hypotheses that best reflect the case summary or problem representation.
- Learning or Working Diagnosis: A diagnosis that has reached a level of probability sufficient for the clinician to initiate further testing or begin treatment, even if it has not yet been definitively confirmed.
- Diagnosis Justification: The process of using key clinical findings to identify the most likely diagnosis or diagnoses, and to justify that selection by comparing and contrasting with alternative possibilities.
- Management and Treatment: The steps taken after the clinical reasoning process, including prognosis, treatment planning, management, preventive measures, and symptom palliation, aimed at improving quality of life—along with the rationale for these decisions.
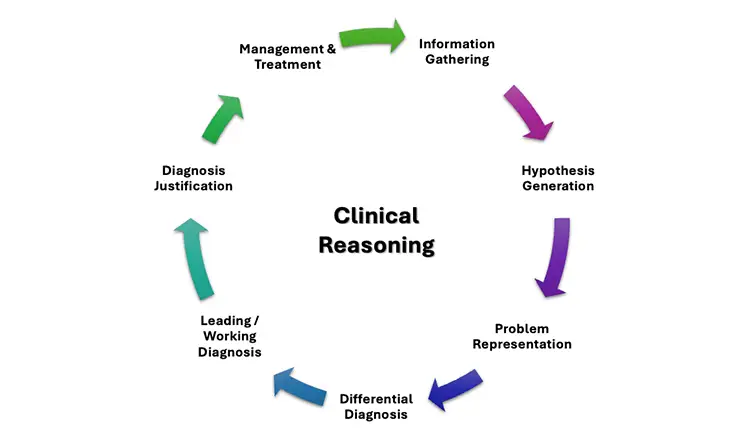
Image 1. Clinical Reasoning Components
Understanding these components is essential for educators designing learning experiences and assessments that effectively develop clinical reasoning skills.
Challenges of Clinical Reasoning Assessment:
Being such a complex construct of teaching, learning, and assessing Clinical Reasoning poses multiple challenges to educators, namely:
- Capturing the reasoning process, which often occurs internally and is not easily observable.
- Lack of standardized definitions and frameworks, making assessment inconsistent.
- Limited authenticity and validity in traditional assessment tools.
- Overreliance on multiple-choice questions (MCQs), which fail to capture the dynamic nature of reasoning.
- Subjectivity and variability in raters’ judgments, especially in open-ended assessments.
- Underuse of longitudinal and programmatic assessment, which are better suited to tracking reasoning development over time.
- Cognitive load issues, especially in high-stakes or unfamiliar scenarios.
- Limited feedback mechanisms, reducing opportunities for reflection and improvement.
- Diverse assessment strategies, leading to inconsistent evaluation.
How can Body Interact Virtual Patients promote Clinical Reasoning Assessment?
Body Interact virtual patients can be used to assess clinical reasoning by simulating realistic clinical scenarios that require students to engage in decision-making processes similar to those used in real clinical environments.
1. Simulation of authentic clinical contexts
By mirroring the complexity and uncertainty of real-life clinical encounters, Body Interact helps students navigate information gathering, hypothesis generation, and problem representation in a safe, controlled setting.
This promotes the assessment of higher-order thinking, cognitive engagement, and critical thinking in ways that traditional assessments (such as MCQs) may struggle.
2. Visualization of reasoning processes
Body Interact can log decision pathways and clinical choices, making the reasoning process transparent. Educators can track how students arrive at their conclusions, providing insight into their diagnostic and management thinking.
3. Scaffolded and repeated practice
Students can revisit cases, reflect on their decisions, and compare alternative approaches. This opportunity for repetitive exposure helps to reinforce learning and build pattern recognition skills essential to expert reasoning.
4. Immediate, contextualized feedback
Virtual patients provide real-time feedback, aligned with the reasoning and decision-making steps taken by the student. This type of feedback supports metacognition and allows students to refine their clinical judgment over time.
5. Rich data for Programmatic Assessment
By capturing detailed student performance data across multiple cases and over time, Body Interact supports longitudinal tracking of clinical reasoning development. This makes it possible to assess progression, identify areas needing support, and integrate clinical reasoning into programmatic assessment frameworks.
6. Team-based and individual skills development
Body Interact provides the grounds for both solo and collaborative decision-making skills development, enabling the assessment of not just individual clinical reasoning, but also team-based reasoning and communication skills.
7. TStandardization and holistic assessment
Integrating resources such as checklists, concept maps, or Think-Aloud protocols for conducting assessments with Body Interact Virtual Patients not only reduces variability between examiners but also promotes educators in capturing the various components of clinical reasoning.


Best Practices for using Body Interact in Clinical Reasoning Assessment
To maximize the effectiveness and educational value of Body Interact, educators should consider the following best practices when integrating it into assessment strategies:
1. Align scenarios with learning objectives
Ensure that each virtual case elicits the specific components of clinical reasoning you intend to assess.
2. Use structured assessment tools
Complement the use of Body Interact with structured rubrics or scoring frameworks (e.g., Script Concordance Tests, Checklists, Oral examinations) to objectively evaluate Students’ reasoning processes.
3. Facilitate reflection and debriefing
After virtual patient encounters, conduct guided debriefing sessions to help students reflect on their thought processes. Prompt them to explain their hypotheses, justify their decisions, and consider alternative approaches.
4. Integrate with other assessment modalities
Use Body Interact as part of a mixed-method assessment strategy, combining it with OSCEs, case discussions, or portfolios to build a comprehensive picture of a student’s reasoning abilities..
5. Provide continuous feedback and opportunities for remediation
By capturing detailed student performance data across multiple cases and over time, Body Interact supports longitudinal tracking of clinical reasoning development. This makes it possible to assess progression, identify areas needing support, and integrate clinical reasoning into programmatic assessment frameworks.
6. Train faculty on interpretation and use of data
Ensure faculty are prepared to interpret and use in a standardized way the data generated by Body Interact and understand how to assess clinical reasoning using technology and simulation-based evidence.
Body Interact provides a valuable and innovative resource for enhancing the assessment of clinical reasoning by addressing many of the challenges faced with traditional methods. Through immersive, realistic simulations and real-time feedback, it enables both educators and students to make the reasoning process visible, measurable, and improvable.
When used alongside structured assessment tools and reflective practices, Body Interact not only supports the development of individual and team-based clinical reasoning skills but also contributes to a more authentic, consistent, and comprehensive evaluation of student progress in healthcare education.
References
Daniel M, Rencic J, Durning SJ, Holmboe E, Santen SA, Lang V, Ratcliffe T, Gordon D, Heist B, Lubarsky S, Estrada CA, Ballard T, Artino AR Jr, Sergio Da Silva A, Cleary T, Stojan J, Gruppen LD. Clinical Reasoning Assessment Methods: A Scoping Review and Practical Guidance. Acad Med. 2019 Jun;94(6):902-912. doi: 10.1097/ACM.0000000000002618. PMID: 30720527.
Epstein, RM (2007). Assessment in medical education. New England Journal of Medicine, 356(4), 387–396.
Eva, KW (2005). What every teacher needs to know about clinical reasoning. Medical Education, 39(1), 98–106.









