Global Network Event - Annual event on Virtual Patients for the Iberoamerican Community (Part II)
On the 15th of November Body Interact team held another edition of the Global Network Event, dedicated to the Iberoamerican Community. Experts joined to share with the audience their insights and experiences regarding the implementation of Body Interact Virtual Patients for teaching and learning in healthcare contexts.
Explore the 2nd part of the article published on our blog – Revolutionizing Medical Education: Virtual Patients in the Iberoamerican Community – diving into the presentations by Professor Jorge Alvarado and Professor Olivia Rodriguez.
Let ‘s take a look!
Speakers Presentations
Jorge Alvarado
MD, MEM

Professor Jorge Alvarado, the dean of the Medical School of Panamerican University, in Guatemala, is a strong defender of the implementation of clinical simulation in pre and postgraduate teaching, believing that this is one of the pillars of innovation and learning in clinical education.
The Panamerican University, in Guatemala, took on the challenge of doing something completely different from what was the standard in terms of curriculum planning in Guatemala. So, they determined to introduce simulation across the curricular map. But, this decision didn’t come without constraints – introduction of digital solutions many times comes with resistances
To start with, the faculty made an assessment of the students that had applied to register for the medical degree. This profile showed that these were students with studying habits that were possibly not ideal, the use of technology could prove to be a constraint and their concept of a Medical curriculum was to some extense traditional.
Eventhought this was the paradigma that the faculty from Panamerican University had, this was the paradigma they wanted to change!
Breaking paradigmas – Simulation as a learning tool is the title of Professor Jorge Alvarado presentation:
The Panamerican University, in Guatemala, took on the challenge of doing something completely different from what was the standard in terms of curriculum planning in Guatemala. So, they determined to introduce simulation across the curricular map. But, this decision didn’t come without constraints – introduction of digital solutions many times comes with resistances
To start with, the faculty made an assessment of the students that had applied to register for the medical degree. This profile showed that these were students with studying habits that were possibly not ideal, the use of technology could prove to be a constraint and their concept of a Medical curriculum was to some extense traditional.
Eventhought this was the paradigma that the faculty from Panamerican University had, this was the paradigma they wanted to change!
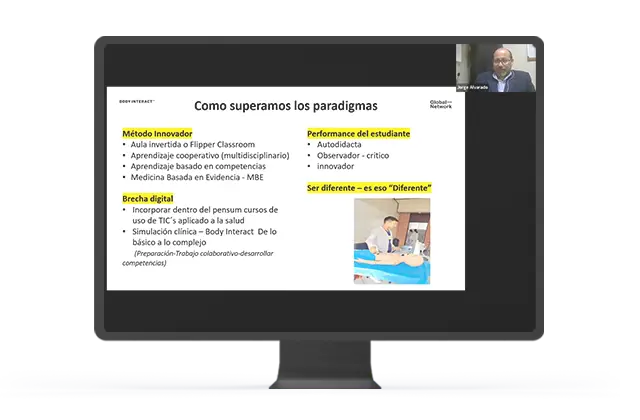
- They applied an innovative method, by implementing in the curriculum Flipped Classroom strategy, Cooperative learning, Competency-based learning and Evidence-based in medicine. Body Interact proven to be a tool that could be efficiently combined with the mentioned approaches;
- To overcome the digital constraints they implemented a course of Technology applied to communication in healthcare;
- They implemented a strategy in which Body Interact is used to explore gradually simple to complex contents.
From this process some outcomes of using Simulation as a teaching resource were mentioned:
- Safer practices and better outcomes
- Better confidence levels shown by students
- Better clinical and critical judgement regarding decision-making
- Reinforced self-guide learning
- Higher demand of professors/specialists skills
Dive into Professor Alvarado’s presentation and take a closer look at the different pedagogical approaches with which Body Interact Virtual Patients was combined!
Ana Olivia Rodriguez
MD

Professor Ana Olivia Rodriguez works as a doctor and professor in the Medical degree of Valle del Mexico University (UVM). She is also the Coordinator for the Clinical Simulation Department in Veracruz campus at UVM.
If you would like to know how Body Interact can be used in clinical training of Medical students in the ealy stages don’t miss Professor Ana Rodriguez presentation:
Explore more here : https://vimeo.com/885589514/2064f62cf2?share=copy
The COVID-19 Pandemia was the driving force behind the large integration of Body Interact Virtual Patient (VP) in the Medical curriculum at UVM.
Body Interact VP were, in the starting moment, used in a more conventional appproach – introducing them to students that were in the stage of clinical rotations.
VP were undoubtedly the way to overcome constraints presented by the lockdowns, providing a way for students to proceed with clinical practice and presenting the right formula to prevent the decay of clinical skills that had already been acquired.
But this was just the beginning, and UVM faculty wondered how they could successfully implement Body Interact VP in the early years of their Medical Curriculum.
Early Clinical Training – Integration in 1st and 2nd years of the curriculum:
- Goal: Integrate basic knowledge and clinical skills to foster clinical reasoning, through the analysis of clinical problems and simulation of clinical gestures and practices in a controlled environment, addressing common pathologies in a gradual way, in order to introduce the student to the clinical method and patient safety, in the primary care level.
- Problem: Students resistance to new teaching approaches
- Intended outcome: Professor Ana Rodriguez mentioned that the integration is considered to be achieved when the educational intention and the continuous practice are capable of creating mental schemes that allows the student to generate and recognize action paterns.
- Process and strategies: The idea behind this integration was to offer a progressive work with Virtual Patients, per mean of a subject of the 1st and 2nd year of the curriculum, that is carried throughout both curricular years.
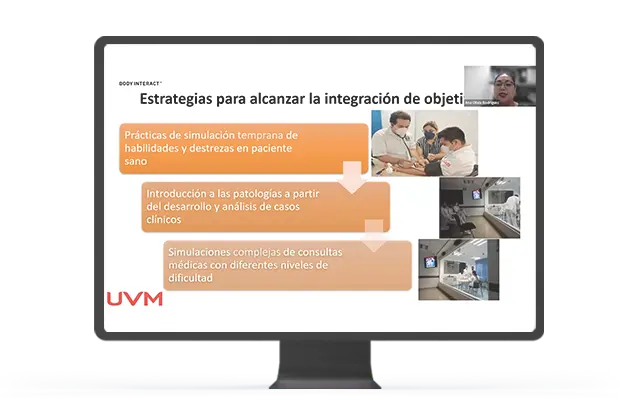
UVM starts by introducing simulation practices focusing on the healthy patient (vital signs assessment, what are the normal parameters, etc). Then they progress into introducing (common) pathologies from the development and analysis of clinical cases (merging for example anatomy concepts and introducing physiology). The last step regards the introduction of complex simulations of medical appointments in different difficulty levels, focusing on topics such as clinical interview, physical examination. Concise and tangible goals are defined gradually for students in this last step.
How does Body Interact activities are introduced to such process?
- The aim of using Body Interact VP in this stage is to start the development of prioritizing skills, making problem analisis, defining patient clinical history, physica examinations, making the analisis of diferential diagnosis and reaching a final diagnosis.

First year students work with VP focusing mainly in physical examination of the patient and doing simple differential diagnosis. VPs with whom these students engage always regard subjects that have been introduced to, with no occult or secondary diagnosis to be defined.
With second year students, the VP is still managed by the tutor but receiving input from the students. In this stage students are able to identify abnormal vital signs and when the status of the patient worsens the tutors uses the pause button to help students to understand the evolution of the patient.Concepts, for example of physiology and microbiology may be merged in the case development, aiming for subjects integration.The initial care of the patient is the focus for VP ate this stage.
Don’t miss the opportunity to see in detail how Body Interact Virtual Patients can be integrated in the initial stage of a Medical curriculum!