Presentation by Professor Henrique Alexandrino
Professor of Surgery in the Faculty of Medicine of the University of Coimbra and Consultant Surgeon (General, Emergency and Hepatobiliary) in Coimbra’s University Hospital Center, Professor Henrique Alexandrino is also an Advanced Trauma Life Support (ATLS) and Definitive Trauma Care (DSTC) instructor and course director, and European Trauma Course (ETC) full instructor. His educational interests include trauma and emergency surgery, as well as teamwork and non-technical skills, both in undergraduate and postgraduate settings.
Maintaining and fostering high levels of medical education during the pandemic was the motto of Professors’ Henrique Alexandrino presentation.
We globally witnessed a clinical education change and challenge during, and with COVID-19, and this event was turned into an opportunity by many educational institutions and teachers, as it was presented by Professor Henrique Alexandrino.
The main limitation imposed by the COVID-19 pandemic in clinical education was felt in terms of on-site learning constraints, which eventually led to a need to adjust teaching, learning, and evaluation methods.
From the speaker’s perspective, some changes will have long-lasting effects in clinical education, such as:
- Limitations in terms of student-patient interactions (ratios and quality)
- Increased share of online curriculums
- Reinforcement of usage of clinical simulation
- Boost of tech apps development for teaching purposes
Virtual Patients were widely used and accepted as a methodology to mitigate the mentioned constraints, and can either be used in self-paced learning, in a guided experience by a tutor, as a group or individual activity, both in live or online classes. As benefits Professor Alexandrino highlighted for the usage of Virtual Patients:
- The flexibility of the tool and cases
- Exposure of students to simulated virtual patients
- Induces immersion
- Active engagement and capture of intrinsic motivation of students unlike many times happens in lectures
And providing and fostering the development of:
Clinical reasoning
Decision-making skills
The speaker highlights the decision-making process as one of the most challenging tasks a doctor has to face, which deciding on the appropriate actions, using evidence as an anchor to that process, and understanding the complexity, uncertainty, and probability in decisions in medical practice is essential.
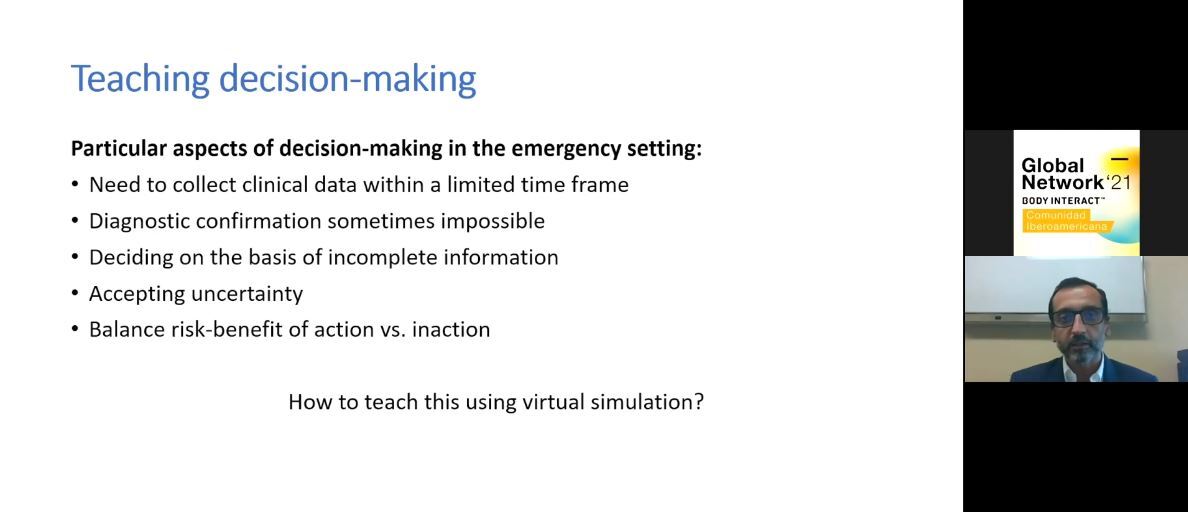
Particular aspects of decision-making in the emergency settings
How can future doctors be taught and trained for future challenges and decisions?
Maybe the answer lies in simulation.
A simulated experience should reproduce reality, have an element of uncertainty, be stimulating, and generate a controlled emotional response. The role of the tutor in this emotional response that a simulated experience produces must be guided so it can be translated into a positive learning momentum, through constructive and structured debriefing.
And, the outcomes and goals of going through a clinical simulation individually or in a tutored way may be set differently.
Professor Alexandrino surveyed his students both on live and online version of this Trauma seminar regarding some points, and students reported:
- An increase in decision-making skills after presential and online seminar using Body Interact;
- An increment in the level of confidence, with no significant differences between online and presential seminar;
- A perception of a higher level of knowledge post-seminar
Professor Alexandrino left us with a couple of interesting take-home messages:
Would you like to get to know more about Professor Alexandrino’s experience with Body Interact virtual patients? Take a look at the recording:
by Daniela Abreu – Body Interact Instructional Designer