Pedagogical Approaches with Body Interact | The Professor Journey
As a professor committed to delivering meaningful clinical learning experiences, integrating Body Interact Virtual Patients into the curriculum transforms how you teach and how students engage with clinical reasoning.
In terms of such integration, there are distinct stages in the effective use of this powerful simulation tool. With this text, we aim to break down the process from a faculty perspective – from initial integration to after-class reinforcement or assessment.
1. The Initial Stage: Laying the Foundation
The first step is embedding Body Interact into the curriculum thoughtfully. In this stage, the work to be conducted includes:
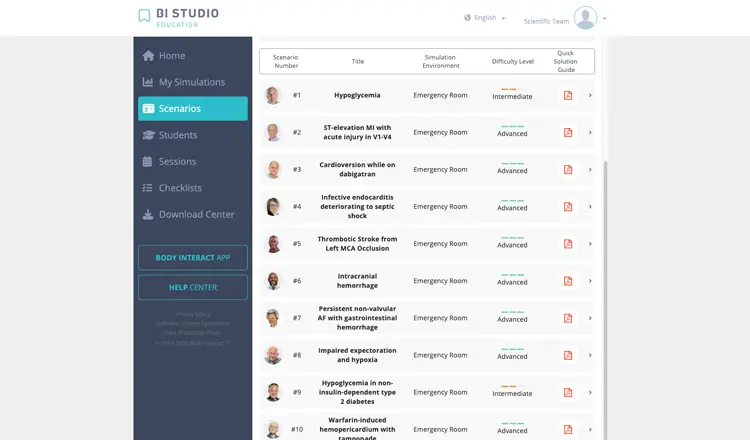
- Case Selection: Choosing cases that are appropriate for the curriculum objectives and level of the students – either to reinforce foundational knowledge for preclinical year students or challenge clinical judgment in senior students.
- Curricular Integration: Mapping Body Interact cases to match learning outcomes, medical specialties, and student levels – ensuring faculty alignment with the use of this simulation resource.
- Faculty Training: Familiarizing professors and technicians with the Body Interact and its Learning Management System – BI Studio – is essential. This training includes understanding the functionality of Body Interact Virtual Patients, analytics, and tools for tracking student performance.
2. Preparing for Class: Building the Clinical Context
Effective simulation-based learning starts before students engage with the virtual patient. Preparation involves:
- Prebriefing Materials: Creating content for students to engage before class with Body Interact, assigning relevant scientific articles, and activating relevant prior knowledge.
- Virtual Patient Setup: Reviewing the chosen Body Interact case and identifying key decision points where student discussion can be encouraged.
3. Conducting the Class: Facilitating the Simulation
Whether delivered in-person or online, Body Interact offers flexibility in pedagogy:
- Pedagogical Approaches: The simulation can be used blended with different pedagogical approaches, like Peer-Assisted Learning, Problem-Based Learning, Team-Based Learning, Hybrid simulation, or Large Group lectures.
- Class Flow: Explore the different class formats and flows – beginning with a briefing, outlining learning objectives and expectations, then moving to the simulation – professor or student-led, individual or group approach.
- Engagement Strategies: Introduce different strategies to promote further engagement.
- Pausing the scenario to stimulate brainstorming, hypothesis generation, and reflective thinking.
- Asking open-ended questions to promote critical thinking.
- Encouraging divergent thinking by discussing multiple clinical pathways or diagnoses.
- Intentionally introducing clinical errors to explore common pitfalls
Promoting such a dynamic structure helps students think like clinicians in a safe, supportive environment.

4. Debriefing: Turning Simulated Experience into Clinical Learning
After the simulation, debriefing is crucial as it helps consolidate knowledge, correct misconceptions, and deepen clinical insight. Depending on the class format:
- Group-Based Debriefing: In a group, conducting reflective discussions on clinical decisions, reasoning processes, and outcomes of the virtual patient.
- Individual-Based Feedback: In individual use, conducting one-on-one feedback sessions, analyzing individual performance, and evolution.
5. After Class: Reinforcing and Assessing Learning
To complete the learning cycle, assign a wrap-up Body Interact case as an asynchronous challenge:
- Wrap-Up Case Assignment: It allows students to self-assess how well they understood the content.
- Performance Monitoring: The case can be used to track progress, highlight areas for improvement, or even contribute to formal assessment.
This final stage encourages students to take ownership of their learning while ensuring they can transfer knowledge to new clinical scenarios.

Initial Stage
– Case Selection
– Curricular Integration
– Faculty Training
Preparing for Class
– Prebriefing Materials
– Virtual Patient Setup
Conducting the Class
– Pedagogical Approaches
– Class Flow
– Engagement Strategies
Debriefing
– Group
– Individual
After Class
– Self-Assessement
– Summative and Formative Assessment
Teaching with Body Interact: A Transformative Approach
Teaching with Body Interact adds an innovative dimension to clinical education practice. By following a structured approach—from planning to post-simulation activities – you can ensure students not only engage but also grow through each clinical encounter.
Simulation is more than a tool; it’s a bridge between theory and practice, helping students become confident, competent future healthcare professionals. So let us help you create engaging learning experiences for your students









